Wisdom Teeth Surgery
The main reasons for removing wisdom teeth are infection, decay, food-trapping, cyst formation, to assist orthodontics, to avoid likely future problems, to avoid more difficult tooth removal when older.
How are they removed?
Wisdom teeth can be removed while you are awake (local anaesthesia/dental injections), sedated (oral or intravenous sedation and local anaesthesia) or asleep (general anaesthesia). The choice depends on the anticipated difficulty of the surgery and also how you would prefer it done. Surgery usually involves raising gum flaps to gain access to the bone which surrounds the tooth. Some of this bone may be removed. The tooth is usually divided up to allow it to be removed in parts. The socket is washed out and the gum closed with dissolving stitches. Upper wisdom teeth are usually easier to remove than lower wisdom teeth. What to expect after:
- Discomfort. Pain-relieving medication is effective and will be required for 5-7 days after surgery.
- Swelling and limited mouth opening. Most obvious 2-3 days after surgery. The majority settles in 4-5 days.
- Bruising. May occur and last for 1-2 weeks.
- Tiredness after general anaesthesia. May be noticeable for several days.
- Nausea or vomiting. May occur but is unusual.
- Weakness of the jaw. For several weeks after.
Some of the risks involved:
- Numbness of the lip, chin or tongue can occur due to the close proximity of two nerves.
This affects about 3% of people having lower wisdom teeth removed and is usually temporary lasting days or weeks. Permanent numbness occurs in much less than 1%. Problems that can result from permanent numbness include lip-biting, reduced awareness of food on the lip, tongue-biting, altered taste, and possibly, altered speech. All patients will experience numbness in the first 24 hrs after surgery due to the local anaesthetic injections given at time of the procedure. - Dry socket.
This occurs in up to 10% of people having lower wisdom teeth removed. The blood clot dissolves a few days after surgery leaving the socket empty (dry) and painful. Normally easily treated. Can be associated with smoking. - Root fragments may need to be left in the tooth socket(s).If the risk of removing them outweighs the benefit. Normal healing can still be expected.
- Infection. Uncommon.
- Excessive bleeding. Uncommon.
- Jaw joint problems. Uncommon.
- Sinus problems. Rare.
Root Canal Treatment
Why do you need a root canal treatment?
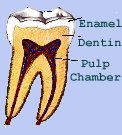
Bacteria, which is the most common cause of infection and inflammation, enters the pulp of the tooth through decay or through a crack. However, other factors may contribute, such as repeated dental procedures, or a blow or traumatic injury to the face. Swelling and discomfort may also occur when toxins from the bacteria leak out of the root end(s) and erode the supporting bone structure leading to an abscessed tooth.
Steps in root canal treatment
 Step 1
Step 1
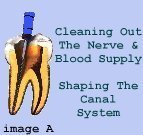
Once a diagnosis has been made, the patient is given local anaesthetic to numb the tooth, thus making treatment very comfortable. A latex sheath called a Rubber Dam is then placed to isolate the tooth being treated, and maintain a clean working field. The dentist then proceeds to access the canals by making an opening and removing all tooth decay.
 Step 2
Step 2
Next the dentist uses a series of calibrated precision hand held instruments called files or reamers to clean and shape the canals. X-rays are then taken throughout the procedure to ensure that the intruments go to the end of the root and not beyond. After the canals are cleaned, shaped and sterilized, they are ready to be filled with a rubbery material called Gutta Percha. The material is injected into the canals and seals off the end of the root preventing any leakage. (*Image B) A temporary filling is placed into the opening, made to access the canals, and the patient is instructed to have this replaced with a permanent filling or a crown by his/her regular dentist.
Dentures
What are dentures? Dentures are artificial teeth that can be removed. Many people who are missing one tooth, several teeth or all their teeth, benefit greatly from denture teeth. Made from the latest polymer resin materials, dentures are very natural looking and they can be matched in color and appearance to your other teeth. Without support from teeth and dentures, facial muscles sag, making a person look older. With dentures, you’ll be able to eat and speak – things that people often take for granted until their natural teeth are gone. A complete denture is for people who have no teeth in their lower jaw or upper jaw, or both jaws. Complete dentures should be removed and cleaned daily to keep your gums healthy and to allow your tissues to relax. Partial dentures are for people who have some natural teeth remaining, or who only need to replace a few teeth. The benefits are the same as for full denture wearers: your facial muscles will be supported, your smile improved and your ability to chew and speak will be enhanced. The dentures should be removed and cleaned daily to keep your gums healthy and to allow your tissues to relax.
Dental Hygienist
What is a Dental Hygienist?
Dental Hygienists (periodontal therapist or gum therapist) are specially trained members of the dental team who work together with your dentist to treat gum diseases and help people maintain good oral health through care of their teeth and gums. Dental Hygienists are strong advocates of the preventative approach to dentistry.
- Do your gums bleed when you brush your teeth?

- Do you ever have pain in your mouth?
- Are you gums red, swollen and tender?
- Do you have bad breath?
- Do you have gums that have pulled away (receded) from the teeth?
- Have you noticed pus between your teeth and gums?
- Are your permanent teeth loose or separating?
If you answered yes to any of these questions you may have a serious infection called ‘Periodontal Disease’, that, if left untreated, can lead to tooth loss.
What is ‘Periodontal Disease’?
Periodontal disease is a slowly progressing chronic inflammation of the gum and the structures that hold the teeth in (bone, periodontal ligament etc). Periodontal disease is made up of two main types:
1. Gingivitis: which is an inflammation of the gums. Your gums become red, inflamed and tender and can bleed when you brush your teeth. It does not include any loss of the structures that hold the teeth in place.
2. Periodontitis: if gingivitis is neglected the inflammation progress may extend deeper into the tissue causing the gum to separate from the teeth, resulting in the formation of a pocket (which act as breeding grounds for bacteria and will eventually fill with pus. The inflammation will extend into the bone surrounding the teeth, which may become loose, drift out of position and will eventually be lost. The terminal stage of this disease used to be referred to as pyorrhea where teeth became loose, surrounded by pus then eventually fell out.
Take the opportunity to see our Registered Dental Hygienist to have your teeth and gums gently cleaned and teeth polished. Simple oral hygiene techniques that you can be taught to use at home will save you money by avoiding preventable problems.
